Blog
-
New technology that can help the 360 million people with hearing loss
 21 Apr , 2017
21 Apr , 2017
New technology that can help the 360 million people with hearing loss
For the 360 million people worldwide who lack some or all of their ability to hear, technological interventions have already come a long way. But still, they’re not perfect.
Soon that might all change. Scientists are working on a number of experimental techniques that may soon transform hearing interventions. That could greatly improve the quality of life for millions, who have been waiting a long time — the last major innovation in hearing technology occurred in 1985.
Normal hearing is more simple than it may appear. Sound waves move through the ear canal and pulse the ear drum, which then moves the tiny bones inside the middle ear. They in turn tap the cochlea, a snail shell–looking structure that contains thousands of delicate hairs and fluid. The cochlea converts mechanical signals into electrical ones, which it then passes to the auditory nerve, which transmits it to the brain for processing.
But the ear presents a difficult engineering problem. If any of these parts are disrupted, a person might lose some or all of her hearing. And what kind of intervention works best depends on which part is affected. Those who lose hearing later in life, either due to a toxin, loud noise or simply as a part of aging, can be fitted with hearing aids to amplify sounds; children born with hereditary hearing loss can get complex devices called cochlear implants surgically placed deep into the ear.
The cochlear implant was approved by the FDA in 1985, and the decades since have offered only incremental improvements on existing technology. Though these technologies have improved millions of lives, the devices are not foolproof. Often, people using them can’t hear as many sounds as people with normal hearing, resulting in big gaps of frequencies used in things like speech or music. Some people choose not to wear hearing aids, because they find them uncomfortable and add little benefit; cochlear implants do come with health risks and have created a rift within the deaf community. For some, none of these interventions work to substantially improve their hearing.
For those who lost hearing later in life, more sophisticated devices might be the first big step to improving hearing. Tobias Moser, a professor of auditory neuroscience at the University Medical Center Göttingen, is working to improve the function of a cochlear implant by turning it into an optical device instead of an electric one. Instead of turning sound into electrical signals to be transmitted to the brain, as current cochlear implants do, this technique turns sound into light. Micro-LEDs flash onto genetically altered neurons, which send the information to the brain.
“This sounds really fancy — it’s very cool — but it’s also not so easy. This is putting optoelectronics into a pretty aggressive environment [in the ear],” said Moser. He and his team have already shown that the device works in rodent models. In the next four years, before it can be tested in humans, they hope to try their technique in other primates and improve the capabilities and hardiness of the device itself.
Other scientists are turning to other senses to encode information usually communicated audibly. “We’re used to thinking that we have five senses, but that’s actually not the case — we have tons of different types of sensory receptors in the body,” said Scott Novich, the co-founder and chief technology officer at start-up Neosensory. The sense of touch, for example, actually processes pressure, pain, temperature and vibration, each through a different type of sensory receptor in the skin, Novich said.
At Neosensory, Novich and his colleagues are developing a commercially available version of VEST, their research project that uses sensory substitution to map sounds onto the skin before the information is transmitted to the brain. Novich’s goal is to make a device that can be worn under clothes and may be more comfortable to wear for long periods of time than hearing aids.
Initial trials show that it takes some time to train the brain to understand these signals, and Novich doesn’t expect VEST to replace hearing aids necessarily — it could compensate for frequencies of sound that hearing aids might not transmit well, or even augment the nuance of information that wearers receive. Neosensory is doing participant research now and hopes to start manufacturing a product in about a year.
Making cells listen
Some researchers are going past devices and working directly on the body’s cells to restore hearing. Stefan Heller, a professor of otolaryngology at Stanford University, is figuring out how to revert inner ear cells to their earlier, functional state in order to restore hearing. It’s an ability that birds have and mammals lack, so Heller and his team have been working to understand how cells tell each other to regenerate. In five to 10 years, they plan to start testing a few drug compounds on humans. If all goes as planned, their discoveries wouldn’t offer a cure for hearing loss but could give people with degenerative hearing loss the option to take a drug and delay getting a hearing aid.
Albert Edge, a professor of otolaryngology at Harvard Medical School, is also looking into regenerating cells to restore hearing. But his lab has focused on the hair cells inside the cochlea and the neurons from the auditory nerve connected to it. Four years ago Edge and his collaborators discovered that certain molecular compounds could help hair cells regrow, which led to an improvement in hearing in mice. That showed them it could be done, but the effect was not as dramatic as they would have liked, said Edge.
Armed with more knowledge about how cells regenerate elsewhere in the body, Edge and his team have been exploring how various drugs can encourage the regrowth of hair cells and neurons. Ultimately, drugs, which would likely have to be injected deep into patients’ ears, could be tailored to individual needs. “What’s attractive about our approach and others like us is that our aim is to restore the ear to what it was,” Edge said. The goal is providing alternatives to people for whom hearing aids are not a good option. Edge’s work is still limited to Petri dishes and mice, but his team hopes to start some small clinical trials in a few years.
For those with inherited hearing loss, many of these approaches won’t work. If a person had a genetic mutation that caused the cochlear hairs to die off, taking a drug like the one Edge is working on won’t fix that problem. “Even if we did regenerate the cells with a drug, they would still be defective and would presumably die off because [the person] would still have the same mutation,” Edge said.
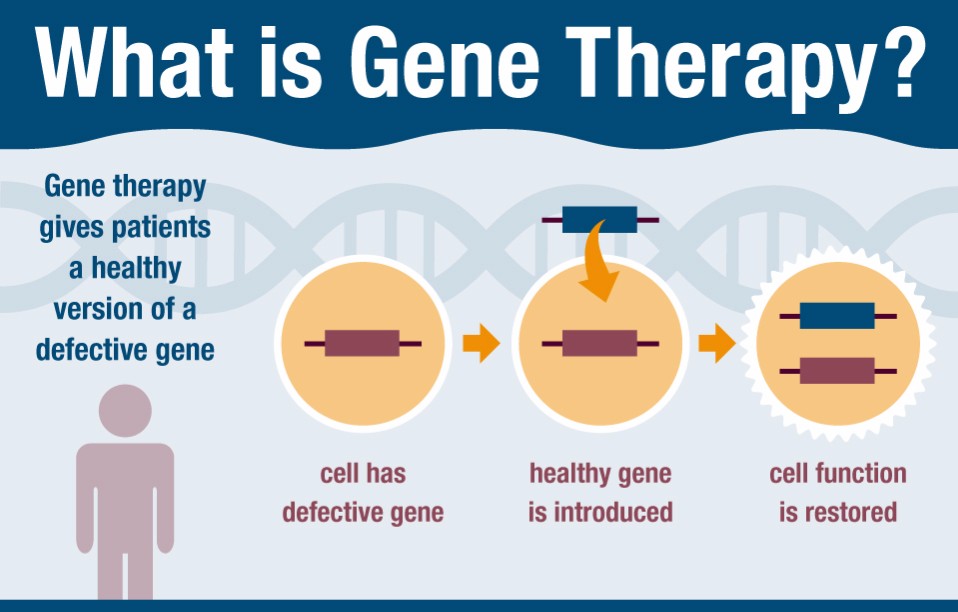
Some researchers are looking into fixing the mutation itself through gene therapy. In experiments, the altered gene is delivered to the relevant cells using a modified virus. That sounds simple enough, but the reality is much more complicated — there are hundreds of genetic mutations that can cause deafness, so researchers have to make sure they’re targeting the right ones and that they’re doing it in the right cells.
The researchers are still figuring out exactly when this kind of therapy would be the most effective (it would likely be at a very young age, as the cochlea degenerates over time in people with hereditary hearing loss). Several researchers, including Moser’s group, have already been able to dramatically restore hearing in deaf mice over a period of several months. But Moser said that because there are so many genes that can cause hearing loss, any specific gene therapy may only be applicable to a small percentage of cases. In order to use gene therapy to make a big dent in the number of hereditary cases, scientists need to have the ability to edit hundreds of genes. That’s not possible with much specificity yet, Moser said.
All these advances can drastically improve the quality of people’s lives, but quick fixes for hearing loss are not coming soon, in Heller’s estimation. “I don’t think there’s something on the horizon, whether it’s a technological device or a drug, that will provide an immediate cure,” he said. Indeed, nearly all the researchers stressed that most of these technologies will not be available to the general public anytime soon. They said press coverage typically leads to dozens of letters from patients volunteering for research into these techniques, and they usually have to tell people in search of hearing help that the techniques are not yet ready.
Heller expects that progress will be step-by-step. First, diagnostics will greatly improve over the next few decades, followed by breakthroughs in hearing aids and cochlear implants, drugs and maybe gene therapy. It’s not clear which will come first, and it could take as long as 100 years, but chances are, the deaf and hard of hearing will have many more options than they do now.
“It’s an exciting time to be working on hearing restoration,” Moser said.
Source: Alexandra Ossola, CNBC.com
Image credit: St Jude Reasearch Hospital